9 reasons why heavy ion therapy is the 2026 choice for pancreatic cancer
In early 2026, the medical community is shifting its focus toward carbon ion therapy as the primary curative path for locally advanced pancreatic cancer, a disease that has long remained resistant to surgery and conventional radiation. New clinical guidelines from the World Oncology Forum now list heavy ion particles as the preferred intervention for tumors that wrap around major blood vessels, where traditional surgical resection is impossible. This change is driven by a decade of trial data showing that the dense ionization of carbon beams can penetrate the thick, fibrous tissue surrounding pancreatic tumors, which typically acts as a shield against chemotherapy.
Overcoming the stromal barrier
The primary challenge in treating pancreatic cancer has always been the "stroma"—a dense layer of non-cancerous cells that protects the tumor. In 2026, carbon ion therapy is being utilized because its high-linear energy transfer (LET) particles can shatter this protective layer. By delivering a lethal dose directly to the malignant core while sparing the nearby stomach and intestines, hadron therapy market centers are achieving local control rates that were previously thought impossible for Stage III patients.
Reducing surgical morbidity through neo adjuvant care
A major trend in 2026 is the use of "down-staging" via particle therapy. By treating patients with carbon ions before surgery, clinicians are often able to shrink a "borderline resectable" tumor away from critical arteries. This makes subsequent surgery much safer and more effective. Reports from high-volume centers in Japan and Italy indicate that patients who receive this sequence of treatment have significantly higher five-year survival rates and a lower likelihood of the cancer returning in the same location.
The precision of MRI guided particle beams
Treating the pancreas is notoriously difficult due to its location and the constant movement of the digestive tract. The 2026 generation of particle accelerators is equipped with integrated MRI-guidance, allowing the beam to "track" the pancreas in real-time. If the organ moves even a few millimeters, the system automatically pauses or adjusts the beam. This level of precision ensures that the high-potency particles do not hit the sensitive duodenum, which has been the primary limiting factor for dose escalation in the past.
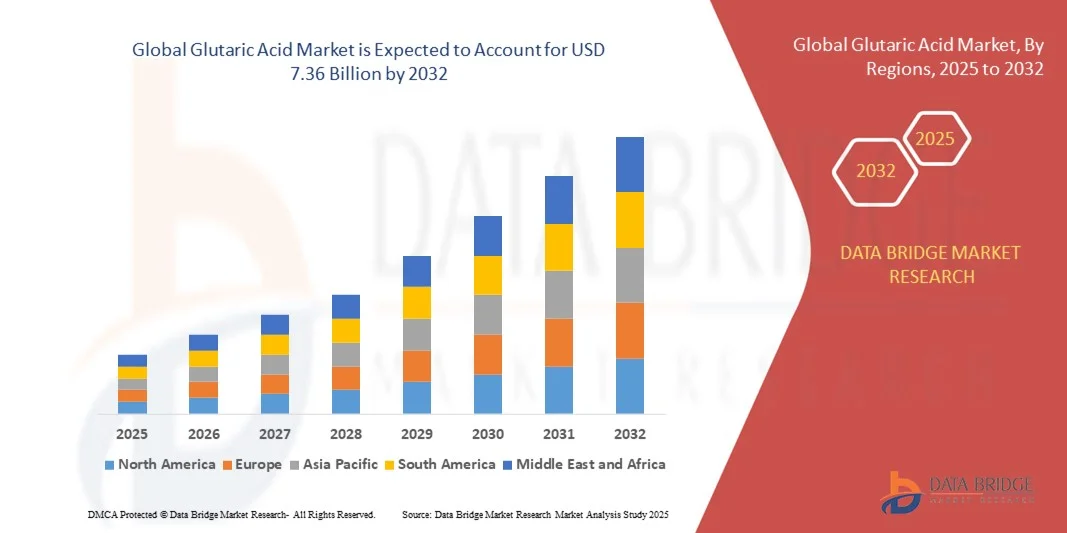
Global expansion of specialized pancreatic centers
Recognizing the success of this approach, several countries are now building dedicated "Gastrointestinal Particle Centers." In 2026, South Korea and Austria have opened wings specifically for the treatment of abdominal malignancies. These centers are staffed by multidisciplinary teams of radiation oncologists, surgeons, and gastroenterologists who specialize in "particle-first" treatment plans. This specialization is expected to lead to a rapid standardization of care and a global improvement in outcomes for one of the world's most lethal cancers.
Trending news 2026: Why the pancreas is no longer the "impossible" organ for radiation
- Spain approves new biologic for Churg-Strauss syndrome management
- Japan launches AI-enhanced colposcopy for early cervical screening
- Germany sees surge in custom-fit oral appliances for sleep apnea
- US dental associations release 2026 guidelines for snoring treatments
- New mobile apps for depression screening enter South American pilot
- Italy implements 3D scanning for chronic wound management in 2026
- Germany approves herbal-biologic hybrid for chronic functional dyspepsia
- France research team develops wearable TENS for migraine prevention
- Italy pioneers preservative-free eye drops for chronic allergic relief
- GCC region experiences high demand for long-lasting dermal fillers
Thanks for Reading — Keep an eye on these specialized clinics as they turn pancreatic cancer from a terminal diagnosis into a manageable surgical condition.